Muscular System
Muscles make up almost half of the mass of a human and is the dominant tissue of the musculoskeletal system, the cardiovascular system, and the walls of all the hollow organs of the body.
The most critical physiological characteristic of muscle is the ability of its cells to transform the chemical energy of ATP into mechanical energy and, thus, produce force. These forces are utilized to produce movements of the body and of fluids or other substances through the internal structures of the body. Muscle tissue also functions in the stabilization of body position, regulation of organ volumes, and the generation of heat as a byproduct of its metabolism.
Types of Muscle Tissue:
The three types of muscle tissue include:
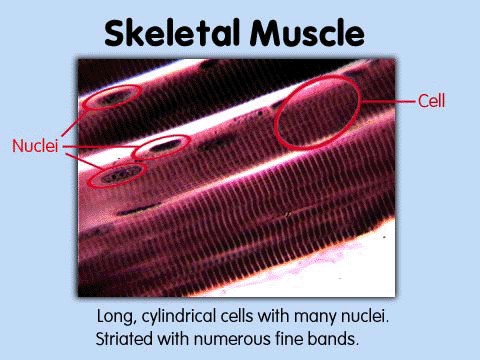
1. Skeletal - primarily attached to the skeletal system; appears striated; under voluntary control.
2. Cardiac - forms most of the heart; appears striated (less than skeletal); under involuntary nervous and endocrine control.
3. Smooth - located in the walls of hollow organs and in the skin; appears smooth or non-striated; under involuntary nervous and endocrine control.
Primary Functions of Muscle:
1. Motion produced by the integrated actions of the bones, joints, and muscles.
Motion produced by the integrated actions of the bones, joints, and muscles.
2. Movement of substances through the body, such as the contractions of the cardiac tissue to pump blood through the circulatory system, or contraction of the smooth muscle in the walls of the gastrointestinal tract to move ingested material through the body.
3. Stabilization of the position of the body and regulation of organ volumes, such as the contractions associated with posture or the utilization of sphincter muscles to control emptying of organssuch as the stomach or urinary bladder.
4. Generation of heat due to cellular respiration.
Characteristics of Muscle Tissue
The five characteristics of muscle necessary for its functions are:
1. Excitability: the ability to respond to stimuli by the production of electrical impulses.
2. Conductivity: the ability to propagate electrical potentials along the plasma membrane of its cells.
3. Contractility: the ability to forcibly shorten.
4. Elasticity: the ability to return to an original length following contractions or extensions.
Anatomy Terms
Deep fascia: Dense, irregular connective tissue that holds muscles together and separates them into functional groups.
Epimysium: The outermost layer of fascia surrounding a whole muscle.
Perimysium: Penetrating from the epimusium, a layer of fascia that surrounds fascicles.
Fascicle: A bundle of between 10 and 100 individual muscle-fibers.
Endomysium: Penetrating from the perimysium, a layer of fascia that surrounds the individual muscle fibers.
Tendon: A cord-like structure of dense connective tissue that connects a skeletal muscle to a bone.
Apneurosis: A broad, flat layer of connective tissue that typically connects skeletal muscle to bone.
Motor neuron: A neuron that innervates a muscle fiber.
Motor unit: A single motor neuron and all of the skeletal muscle fibers in innervates.
Synapse: A specialized region of plasma membrane and the space between them that serves as a point of communication between excitable cells.
Neurotransmitter: A general term for the chemical released by excitable cells which will alter the electrical potentials of the target cells.
Myoneural junction: A synapse between a motor neuron and a skeletal muscle fiber.
Acetylcholine: The sole chemical messenger used at the neuromuscular junction of skeletal muscle.
Motor end plate: A specialized area of muscle fiber plasma membrane containing acetylcholine receptors.
Micro Anatomy
The three types of muscle fibers are:
1. Type I (slow oxidative) - have the smallest diameter; contain large amounts of myoglobin and many mitochondria; well supplied with capillaries; appear red in color; have the capacity to generate ATP primarily using the aerobic system; resistant to fatigue; produce a slow contraction velocity.
2. Type IIa (fast oxidative-glycolytic) - intermediate diameter; large amounts of myoglobin; many mitochondria; well supplied with capillaries; appear red in color; generate ATP through both aerobic and anaerobic systems; produce higher contraction velocity than type I fibers; less resistance to fatigue that type I fibers.
3. Type IIb (fast glycolytic) - largest diameter; low myoglobin content; few mitochondria; poor capillary supply; appear white in color; generate ATP by anaerobic systems; contraction velocity is high; poor resistance to fatigue.
Cardiac v. Skeletal Muscle
Cardiac muscle fibers are striate, having the same basic arrangement of sarcomeres as found in skeletal muscle, but are shorter in length and larger in diameter. Unlike skeletal muscle fibers, cardiac muscle fibers exhibit branching and are uninucleate. They have a less extensive SR system than is found in skeletal muscle and as such must utilize extra-cellular calcium as part of their contraction process. The slower deliveryand removal of calcium across the sarcolemma produces a prolonged contraction and refractory period. Cardiac cells utilize aerobic systems for the production of ATP almost exclusively and must be well supplied with oxygen and thus have extensive capillary networks (from the coronary artery system). Unlike skeletal muscle fibers which are insulated from one another, cardiac muscle fibers are connected to one another at the ends of adjoining fibers by an intercalated disk of the sarcolemma. This contain many gap junction which facilitate the spread of the muscle action potential from one fiber to the next, allowing for the spread of electrical excitation across the tissue.
Muscle Fiber
Striped muscle
Skeletal muscle movements
The origin of a muscle is the point of attachment of that muscle tendon to the relatively stationary (fixed) bone during contraction of the muscle. The insertion is the point of attachment to the relatively movable bone. The action of a muscle is the description of the type of movement that occurs at the joint it controls.
Smooth Muscle
Smooth muscle tissue is either visceral (single-unit) or multi-unit. Visceral is the most common form wrapped around the walls of hollow organs. The fibers of this muscle are connected by gap junction to allow the spread of electrical excitation from fiber to fiber. Multi-unit fibers are found in arrector pili muscles of hairs and in the large airways of the lungs and in large arteries. Each fiber has its own motor neuron and excitation typicallyresults in the contraction of single units.
Smooth muscle fibers are spindle shaped, have a central nucleus, and display no striations. Smooth muscle fibers do contain both thick and thin myofilaments, but they are not arranged in regular sarcomeres. In addition, smooth muscle fibers contain intermediate filaments attached to structures called dense bodies that are dispersed throughout the sarcoplasm as well as anchored to the sarcolemma. During contractions, the sliding action of the thick and thin filaments is transferred to the intermediate filaments and thus to the dense bodies attached to the sarcolemma causing a shortening of the distances between carious portions of the sarcolemma.
Gross Anatomy
Head
Shoulder
Forearm
Back
Abdomen - Thorax
Pelvic
Leg (anterior)
Leg (posterior)
Contraction
Excitation-contraction coupling refers to the relationship between the electrical events on the sarcolemma of muscle fibers, which are excitable cells, and the forceful contractions of the sarcomeres of the muscle fibers. The electrical excitation of the sarcolemma, when propagated as a muscle action potential, will trigger events inside the cell which will result in the development of contractions.
The resting membrane potential is an electrical potential that exists across the plasma membrane of cells. In muscle fibers, the sarcolemma is a selectively permeable membrane. Primarily through theutilization of membrane channels and sodium/potassium membrane pumps, considerable differences in the concentrations of cations and anions can be produced between the external and internal fluid compartments (extracellular vs. intracellular) resulting in a measurable voltage or a polarized membrane.
A muscle action potential is a rapid change in the resting membrane potential, called a depolarization, that can be propagated along the cell membrane, in this case the sarcolemma. It is produced by the release of acetylcholine from the innervating motor neuron. This neurotransmitter is released into the synaptic cleft of the myoneural junction and diffuses across to waiting acetylcholine receptors at the motor end plate. The binding of acetylcholine at the motor end plate opens chemically-mediated sodium channels, resulting in a rapid flow of sodium across the sarcolemma as it follows its chemical and electrical gradients. This ionic binding of acetylcholine at the motor end plate opens chemically-mediated sodium channels, resulting in a rapid flow of sodium across the sarcolemma as it follows its chemical and electrical gradients. Thisionic current opens voltage-mediated sodium channels along the length of the sarcolemma, propagating the potential all along the length of the muscle fiber. This electrical event is carried into the muscle fiber along the T-tubules, which are invaginations of the sarcolemma that run deep into the cell.
Calcium concentrations in the sarcoplasm are responsible for the movement of the filaments. Increases in the calcium concentration in the sarcoplasm starts the filaments sliding, decreases turns them off. When a muscle is relaxed (not contracting) there is a relatively low calcium concentration in the sarcoplasm because the sarcoplasmic reticulum (SR) membrane contains calcium pumps that actively move calcium from the sarcoplasm into the SR utilizing ATP to power these pumps. Calcium is sequestered primarily in the terminal cisternae near the transverse (t) tubules. The cisternae of the SR contain a protein called calsequestrin which acts as a binding site for calcium.
The release of calcium for the ST occurs as the muscle action potential is propagated along the sarcolemma and into the T-tubule system, opening voltage-gated calcium channels in the SR membrane. The calcium binds to troponin, altering the shape (denaturing) the troponin-tropomyosin complex. This uncovers the binding sites on the actin molecules to allow for the chemical bonding with the globular heads of the myosin molecules producing actomyosin.
ATP acts to "power" the contraction. The physical shortening (or production of mechanical forces) actually occurs due to shape changes in the myosin heads as they form, break, and reform bonds to the actin filament. The myosin heads contain binding sites for ATP, and when ATP is available and bound to the myosin head it is said to be in a high energy configuration. Immediately upon the binding of the high energy myosin head to actin, the ATP breaks down to ADP and an organic phosphate. As these particles are released, the myosin head changes shape, producing a "ratcheting" movement or power stroke as the head swivels toward the center of the sarcomere. This action draws the actin filament past the myosin filament toward the H zone, effectively producing a mechanical shortening (force). The low energy process of shortening continues.
Relaxation occurs with the cessation of the muscle action potential. Acetylcholinesterase in the synaptic cleft of the myoneural junction rapidly degrades acetylcholine, causing its effect to be short-lived. The muscle action potential ends, the membrane pumps of both the sarcolemma and SR membrane actively move ions to re-establish the resting membrane potential across the sarcolemma and to actively sequester calcium in the SR. With the calcium concentration in the sarcomere reduced, the troponin-tropomysin complex regains its resting shape, covering the binding sites on actin and effectively preventing crossbridge formation. The sarcomeres then returns to their resting lengths.
Tension Production
A muscle twitch is a contraction of all the muscle fibers in any single motor unit in response to a single action potential from its motorneuron. A graphic record of this response is a myogram. A myogram will show three components:
1. Latent period which shows a slight delay between the delivery of the stimulus and the production of appreciable force. This is due to the time necessary for the delivery of calcium from the SR and time necessary to take the "slack" out of the myoelastic component of the muscle.
2. Contraction period, in which forces increase as the sarcomeres attempt to shorten.
3. Relaxation period, in which forces decrease following the cessation of the stimulus and the resetting of the muscle resting potential and the sequestering of calcium.
Frequency of Stimulation
Refractory period is a brief period of lost excitability in excitable cells due to the time required to re-establish necessary membrane potentials to propagate impulses. In muscle fibers it varies for about 5msecs in skeletal muscle to 300msecs in cardiac muscle.
Temporal summation is the phenomenon of a differential response to two identical stimuli applied in rapid succession. If a stimulus is applied, followed by a second identical stimulus that is applied quickly after the first, but delayed enough to occur following the refractory period, the response to the second stimulus will be greater than the first.
Tetanus is a sustained muscle contraction that occurs when the stimuli are applied so rapidly that the muscle fibers cannot relax prior to the arrival of the next stimulus. In such a case, calcium is being released much more rapidly that it can be actively sequestered, resulting in continued contraction.
Treppe is a "stairstep" increase in the force of contraction that occurs in muscle fibers with successive identical stimuli that are too far apart for temporal summation to be acting. Once again, although the stimulus are not applied rapidly enough for tetanus to occur, they are still being produced at a frequency that does not allow all the calcium to be sequestered prior to the next stimulus, resulting in slightly increased contractions with each stimulus applied.
Length-Tension Relationship
The length-tension relationship of a muscle is related to the overlap between the actin and myosin filaments. In order for contractions to occur, some overlap between these filaments is required. If a muscle were overstretched to the point that the myosin and actin did not overlap, no crossbridges could be formed and thus no contraction would be possible. A muscle will produce the maximal contraction force when an optimal overlap occurs at an optimal length. Increase or decreases in the optimal length will result in lowering the force of contraction.
Motor Unit Recruitment
The primary control of forces produced in a muscle is through motor unit recruitment. Muscles are composed of motor units, each consisting of a single motor neuron and all the muscle fibers that it innervates. Each motor unit will produce force an an "all or none" phenomenon. When activated, each muscle fiber will maximally contract. To alter the amount of contraction force in whole muscles, different numbers of motor units can be activated, recruiting additional motor units as greater and greater forces are required.
Types of Muscle Contractions
Isotonic contractions occur when movement at a joint occurs. In other words, an isotonic contraction is one in which the force produced by the muscle is either greater or lesser that the external load placed on the muscle. Isotonic contractions can be either concentric, in which the force produced is greater than the external load such that the muscle will shorten, or eccentric, in which the force produced is less than the external load such that the muscle will lengthen. Isometric contractions are those in which no movement occurs at a joint. In this case, the amount of force produced in the muscle must exactly equal its external load.
Muscle Metabolism
The three metabolic systems that provide ATP for muscle contractions are the phosphagen system, the anaerobic system (glycogen-lactic acid) and the aerobic system. The phosphagen system provides energy when muscles are contracted maximally. This system utilizes stores of existing ATP and creatine phosphate (CP), a molecule that can transfer its high energy phosphate unit directly to ADP. Together, ATP and CP can provide approximately 10-15 seconds of energy during its maximal use. The anaerobic system is also a rapid producer of energy., utilizing glycolysis to provide ATP. It is limited by the ability of the cell to tolerate lactic acid accumulation, byproduct of these reactions. When energy metabolism occurs more rapidly than oxygen can be delivered to the cells, lactic acid accumulates. Typically, anaerobic metabolism can supply about 30-40 seconds of maximal muscle activity prior to the critical accumulation of acidity. The aerobic system utilizes cellular respiration and can provide theoretically unlimited energy provided that the pace of energy production can be matched to the delivery of oxygen, resulting in the production of pyruvic acid rather than lactic acid, Unlike lactic acid, pyruvic acid can be further metabolized in the mitochondria of the muscle fibers so that no appreciable acidity builds up.
Muscle Fatigue
Muscle fatigue occurs due to a number of factors, but truly results when there is insufficient ATP to meet the needs of contracting muscles. The factors include insufficient oxygen (which leads to the accumulation of lactic acid), insufficient glycogen (glucose), or failure of motor neurons to release acetylcholine. Delayed onset muscle soreness is often mistakenly associated with a buildup of lactic acid in the muscle. Approximately 80 percent of lactic acid produced in muscles diffuses out of the muscle immediately upon production. The remaining 20 percent is rapidly metabolized when muscles come to rest. Muscle soreness after intense bouts of exercise occurs due to the accumulation of fluid (swelling) in the muscle that results from microscopic damage to the myoelastic components of muscles during sustained large contraction.
Leverage
A lever is defined as a fixed rod that moves (rotates) over a fixed point called the fulcrum. A mechanical advantage, called leverage, is gained by the use of a leer. The musculoskeletal system is a system of levers in which bones act as levers, joints acts as fulcrums, and muscles supply forces. First class levers have the fulcrum between the force and the resistance and are relatively rare in the body. An example of a first class lever would be extension at the atlanto-occipital joint. Second class levers have the fulcrum at one end with the force applied at the other end and the resistance between them. Again, this is relatively rare with plantar flexion of the foot as an example. Third class levers have the fulcrum at one end and the resistance at the opposite end with force applied between. This is the most common lever of the body with flexion at the elbow as an example.
Muscle Architecture
Muscle fascicles can be arranged in the following pattern:
1. Parallel - fascicle are parallel to the longitudinal axis of the muscles and terminate in aponeuroses. They have relatively few fascicles distributed over the aponeurosss and thus produce greater range of motion than power.
2. Fusiform - fascicles are also nearly parallel to the longitudinal axis of the muscle but terminate in tendons, producing a "tapering" of the muscle from the thicker central belly to the tendons. This produces a larger number of fascicles distributed over the tendon and produces a balance of range of motion and power.
3. Circular - fascicles are in concentric circles with the origin and insertion near the same point producing a sphincter to enclose an opening.
4. Pennate - fascicles are short in relation to the muscle length and attach obliquely to the tendon, providing a very large number of fascicles distributed over the tendon, producing great power but a relatively smaller range of motion.
Review Questions:
1. List the three types of muscle tissue and identify the general location, anatomical characteristics, and nervous or endocrine control differences among them.
2. List and describe the four primary functions of muscle tissue.
3. List and briefly describe the five principle characteristics of muscle tissue required for its functional capabilities.
4. What is a muscle action potential?
5. What is a resting action potential?
6. What is the role of ATP in muscle contraction?
7. What is the role of calcium in muscle contraction?
8. What is a muscle twitch?
9. How does a muscle relax?
10. How is the force produced by a muscle controlled?
11. What is the difference between isotonic and isometric contractions?
12. What are the three metabolic systems by which muscle fibers produce ATP?
13. List and describe the three muscle fiber types?
14. How is cardiac and skeletal muscle tissue alike and different?
15. What are the two type of smooth muscle tissue and how do they differ?
16. What is the difference between the origin and insertion of a muscle?
17. Describe the arrangements of fascicles and their functional significance.
18. What produces muscle fatigue?
19. What produces muscle soreness following intense exercise?
20. Describe the microscopic anatomy of smooth muscle.